
Rapid growth and development can expose a society to newly emerging and re-emerging health issues and global public health threats. Lags in innovation in medical science and healthcare technology, increases in the vulnerable ageing population, and inadequate healthcare resources can exacerbate these issues. Various studies have shown that coupled with chronic disease, the prevalence of diabetes, hypertension, coronary heart disease, and chronic obstructive pulmonary disease is at an all-time high (Vij 2022; Pribish et al. 2019; Standl et al. 2019).
Challenges in health inclusion
Medical science considers diabetes a gateway to many chronic conditions. Figure 1 shows the age-adjusted prevalence of diabetes across regions. The problem is poignant in developing and less-developed countries, which are experiencing increasing pressure due to their aging populations and decreasing mortality rates (Kelly and Fuster 2010). Healthcare issues in developing and less-developed countries are known as the “triple A,” comprising problems pertaining to availability, accessibility, and affordability (Mishra and Sharma 2022). Therefore, rectifying the uneven distribution of healthcare (Deutsch et al. 2020) and access to healthcare remains key to reducing health inequity.
Figure 1: Age-Adjusted Comparative Prevalence of Diabetes (%)
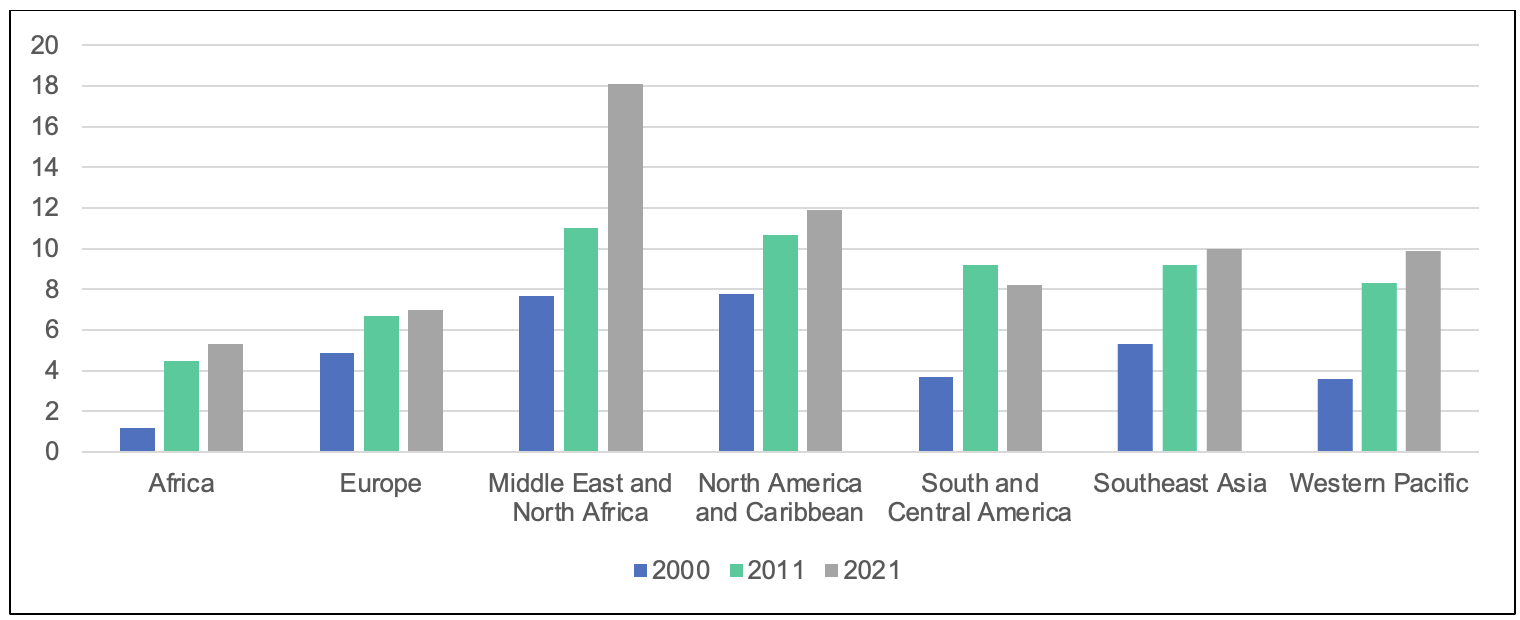 Source: Diabetes Atlas.
Source: Diabetes Atlas.
The continuous development of healthcare calls for genome testing to tailor drug choice and dosing depending on a patient’s genetic makeup. Consequently, better healthcare requires an enormous investment in healthcare facilities. However, in sparsely populated rural areas, income inequality and the large distances from facility centers hinder efforts to provide improved healthcare as investors find no viable business proposition. Moreover, small and medium-scale healthcare providers face challenges in commissioning new technologies in their facilities due to the high cost of advanced instruments, which requires adopting price skimming strategies, resulting in further health inequity. The advent of digital technology addresses these issues through servitization as an economically viable solution.
Servitization of digital healthcare technologies
Servitization provides the option to purchase treatment using capital-intensive medical devices as a service (pay per use) instead of procuring the device itself. Including small players as service providers through servitization allows access to treatment for a large population segment instead of restricting the facilities to a select few. Moreover, servitization can stimulate healthcare technology innovation by building a patient database and designing a stable revenue stream for equipment manufacturers. While digital servitization in healthcare is in its infancy and medical technology firms are struggling to develop and commercialize digital services, researchers consider servitization a viable solution for healthcare inequality.
Increasing attention on digital healthcare servitization brings opportunities and potential. Healthcare emphasizes achieving a desired outcome over specific product or service development, and a focus on servitization can facilitate meeting this objective. Figure 2 depicts the route of servitization in healthcare, where buyers and sellers move from products to outputs to outcomes. Outcome-selling focuses on the buyer’s desire rather than the products or services the seller offers. It encourages conversion by prioritizing the patient’s desired outcome. The prerequisite of this outcome-selling is patient feedback and engagement through two-way communication. This servitization, in turn, increases customer engagement and evokes innovation in business models while continuing to provide healthcare facilities to all.
Figure 2: Ideal Route of Servitization in Healthcare
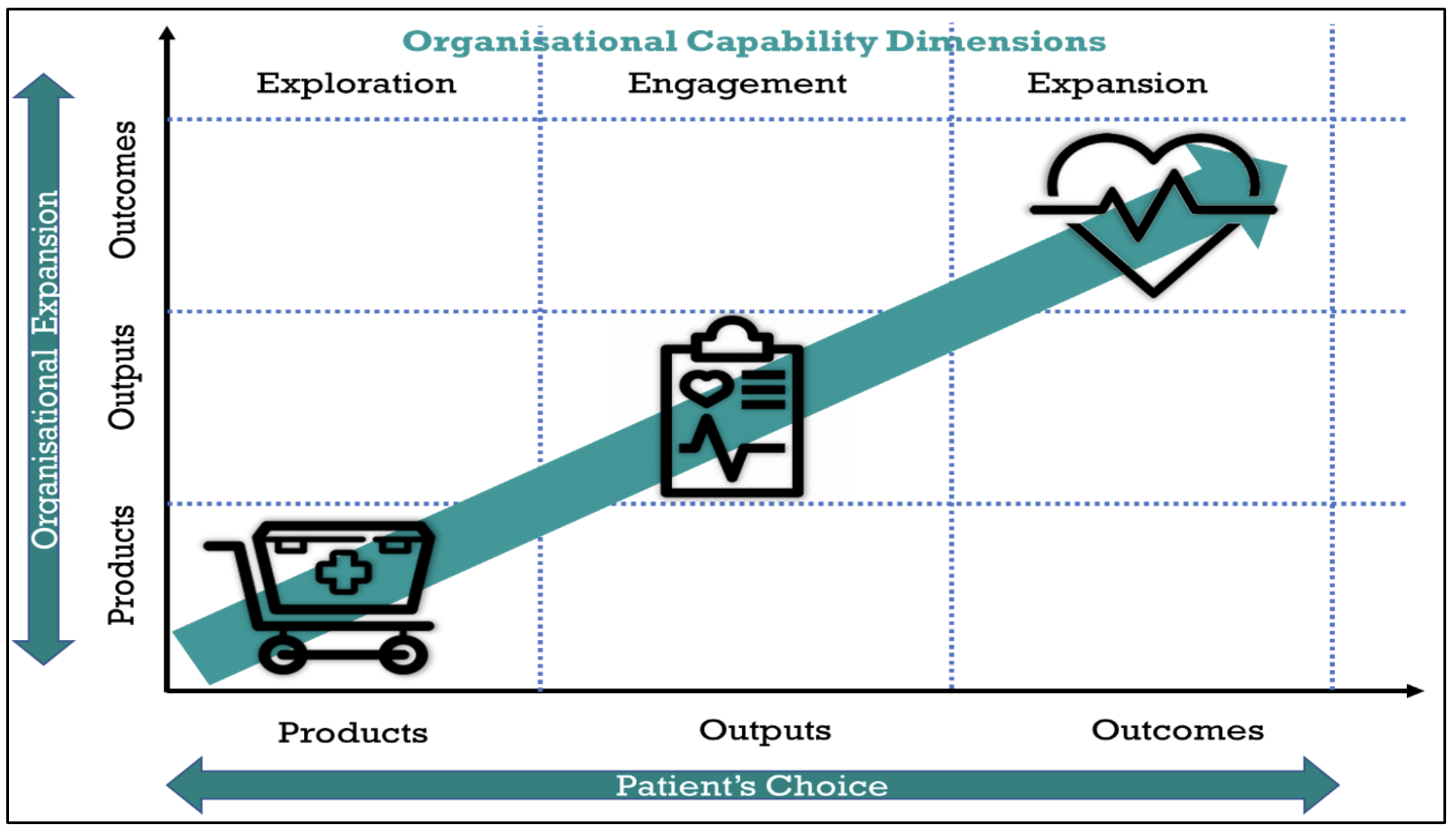 Source: Adapted from PA Consulting (2017).
Source: Adapted from PA Consulting (2017).
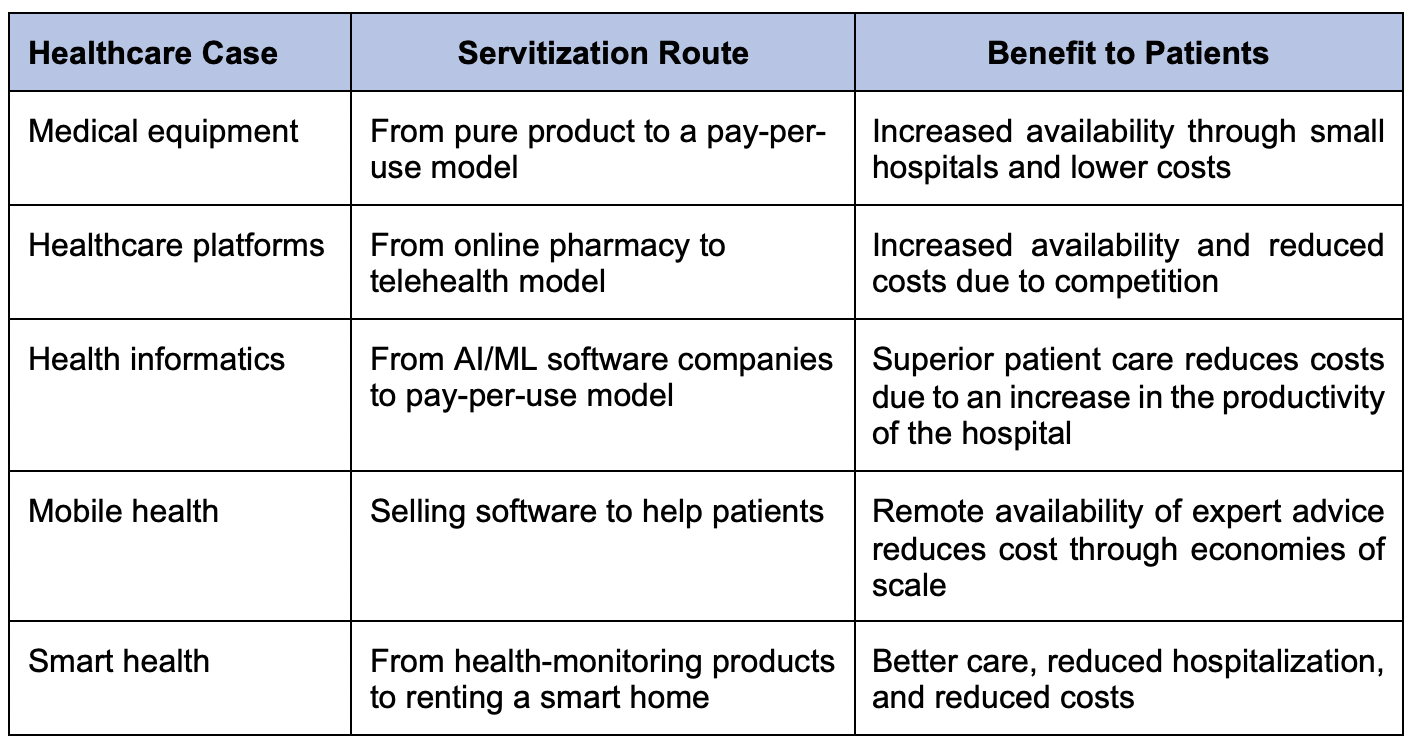
Although the movement from product- to outcome-based healthcare facilities can incorporate servitization in multiple ways, focusing on five major dimensions can bridge healthcare inequalities.
- Servitization of medical equipment
Medical equipment manufacturers can adopt servitization strategies for their expensive products. Original equipment manufacturers (OEM) can offer machines (such as dialysis machines) through a pay-per-use model to small hospitals with financial resource constraints. This strategy can help small hospitals generate revenue through service charges, and patients can access healthcare facilities at a lower cost. Therefore, lower business risk and a broader customer base can further reduce the cost of technology, resulting in health inclusion.
- Servitization of healthcare platforms
Increasing internet penetration and declining smartphone prices have led to fierce competition in the e-pharmacy sector. As part of diversification strategies to increase profitability, e-pharmacies have introduced teleconsulting, benefiting from increased customer loyalty and sales of their medicines (other than over-the-counter drugs). The popularity of this model has surged during the pandemic, and it has become a part of life. Tata 1mg and PharmEasy operate the model in India, while Practo exhibits a presence in India, Indonesia, the Philippines, Singapore, and Malaysia.
- Servitization of health informatics
To provide health informatics to all stakeholders (such as consumers, caregivers, communities, and researchers), tech giants IBM and Google are focusing on artificial intelligence (AI) and machine learning (ML)-based detection, identification, and consultation systems. After the initial offering of the service of its products through its server, IBM Watson Health has shifted to offer AI/ML capabilities on a pay-as-use basis, resulting in a significant decrease in healthcare costs for cancer patients. Google also aims to provide health information to all stakeholders, as access to the latest developments in healthcare is key to providing better services. These readily available technologies augment the work of clinicians and researchers, which reduces the cost of healthcare operations and clinical research.
- Servitization of mobile health
The availability of smartphones at lower prices has brought opportunities for app developers. Although there has been a dramatic rise in the number of mobile healthcare apps, many pose risks in the form of cyber security threats, the misreading of health data, and the security of personal information. The implementation of mobile healthcare app regulations (Islam et al. 2022) can facilitate better customer service with various options, such as the self-management of diabetes and mental health, exercise recommendations, medical nutrition therapy, and medication adherence.
- Servitization of smart health
One of the biggest challenges in providing better healthcare is the continuous monitoring of patients, especially those with chronic diseases and geriatric patients (Mishra and Madakam 2022). Internet of Things (IoT)-based devices can detect and record vitals (such as ambulatory blood pressure) and synchronize data with caregivers and health service providers. Although the possibility of replacing existing healthcare services with IoT-based devices is remote, IoT-based devices can create connected smart homes to enhance the quality of health services.
Digital healthcare servitization is still at a nascent stage, but there is no doubt that systematic implementation can enhance the scope and opportunities for reducing health inequality. Table 1 provides a summary of the servitization of digital health technologies.
Table 1. Healthcare Servitization Examples
 Source: Authors.
Source: Authors.
Policy recommendations
Digital technologies, such as mobile, analytics, cloud, and IoT, are currently driving servitization in the healthcare sector. As shown in Table 1, these healthcare interventions solve the dual problem of availability and affordability and contribute toward health inclusion. The adoption of these services with provisions for tax exemptions and insurance coverage can foster health inclusion. Moreover, subsidized loans to OEM companies in healthcare through priority lending can encourage the innovation of new digital healthcare products and services. The role of the government in the healthcare system is crucial, especially in implementing restrictions and regulations. Governments can support medical equipment companies in offering products as a service after receiving the competent authorities’ approval to safeguard patient safety.
Moreover, digitalization risks the privacy and security of health information. Therefore, governments must ensure patient data security and privacy through robust regulations and customized versions of the Health Insurance Portability and Accountability Act. Undoubtedly, the systematic implementation of the servitization of digital health technology can reduce health inequity.
References
Deutsch, J., J. Silber, G. Wan, and M. Zhao. 2020. Asset Indexes and the Measurement of Poverty, Inequality, and Welfare in Southeast Asia. Journal of Asian Economics 70: 101220.
IDF. 2022. Diabetes Around the World in 2021 (accessed 4 September 2022).
Islam, S. M. S., V. Mishra, M. U. Siddiqui, J. C. Moses, S. Adibi, L. Nguyen, and N. Wickramasinghe. 2022. Smartphone Apps for Diabetes Medication Adherence: Systematic Review. JMIR Diabetes 7(2): e33264.
Kelly, B. B., and V. Fuster, eds. 2010. Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health.
Mishra, V., and S. Madakam. 2022. Smart Healthcare and IoT Technologies: Academic and Service Provider Review. Internet of Things and Data Mining for Modern Engineering and Healthcare Applications (pp. 15–28). Chapman and Hall/CRC.
Mishra, V., and M. G. Sharma. 2022. Telemedicine as Frugal Intervention to Health Care: A Case of Diabetes Management. International Journal of Healthcare Management 15(2): 165–170.
PA Consulting. 2017. Embrace the Benefits of Servitization.
Pribish, A., N. Khalil, R. Mhaskar, L. Woodard, and A. S. Mirza. 2019. Chronic Disease Burden of the Homeless: A Descriptive Study of Student-Run Free Clinics in Tampa, Florida. Journal of Community Health 44(2): 249–255.
Standl, E., K. Khunti, T. B. Hansen, and O. Schnell. 2019. The Global Epidemics of Diabetes in the 21st Century: Current Situation and Perspectives. European Journal of Preventive Cardiology 26(2 suppl.): 7–14.
Vij, V. 2022. Integration of Lifestyle Medicine into the Medical Undergraduate Curriculum. Journal of Advances in Medical Education & Professionalism 10(2): 133–134.









Comments are closed.