
Over 50 years ago, a pioneering medical system was launched in the People’s Republic of China (PRC). Known as the “barefoot doctors” scheme, the program liberalized healthcare beyond doctors and allowed some 1.5 million community health workers to practice basic medicine after 3–6 months of training. This effectively created a national network of healthcare services for the very first time, increasing rural healthcare coverage to 90%. The infant mortality rate in rural areas of the PRC fell over tenfold between 1949 and 2008, while the maternal mortality rate for the same period decreased from 150 women per 100,000 to 41.3 (World Health Organization 2020).
Today, this low-cost, high-performance strategy is back in the limelight as an inspiration for new models of care delivery amid perennial health worker shortages and widening health inequities. The current coronavirus disease (COVID-19) pandemic has also formed a turning point for healthcare digitalization. It has catalyzed unprecedented demand for remote health solutions as face-to-face doctor visits have become risky or impossible—and physicians and patients are finding out that they work (Sayburn 2020).
How can the world expand access to essential health services without emptying government coffers, and where will the healthcare workers come from? Digitalization is not a silver bullet or a cure-all panacea, but it can be a powerful enabler of universal health coverage.
Barefoot doctors 2.0: Technology-driven primary care
Yesteryear’s barefoot doctors were equipped with only a small bag of basic medicines, two syringes, and 10 needles. Today, we can do much more. Modern toolkits for the 21st century barefoot doctor will be built around smartphones, which offer internet access with the attendant benefits of cloud computing and artificial intelligence (AI)-driven decision support. Think of it as “high touch” and “high reach”, the intimacy of a familiar, trusted face with the power of the world’s knowledge at the bedside.
What then, are the must-haves, the essential diagnostic components for a “barefoot doctor 2.0” toolkit?
A typical equipment checklist for general practice clinics lists over 50 essential items, but digitally enabled toolkits can be much leaner. Easy-to-operate, one-stop-shop devices will be integral for facilitating ease of travel.
Some devices on the market fit the bill. TytoHome, a small home examination device, consists of a digital camera, infrared thermometer, otoscope, stethoscope, and tongue depressor adaptor—enough to diagnose many common conditions (Azevedo 2020). For more complex testing functions, we can look to WeDoctor’s Intelligent Health Terminal (see Photo), a portable all-in-one device serving nearly 10 million grassroots users in the PRC. Weighing just 11 pounds, the device can run 11 tests, from routine blood analysis to electrocardiogram (ECG) and early pregnancy tests (see Table) (Dai 2018).
Photo: The Intelligent Health Terminal by WeDoctor

Source: Dai (2018).
Cardiology assessments may be supplemented by InstaECG, an AI-powered device that provides ECG interpretation within 10 minutes (Tricog 2020), while smart intrapartum monitoring tools and portable cardiotocography (CTG) devices from Janitri Innovations could cover maternal assessments (Janitri Innovations 2020). As with the TytoCare model, test results from all these devices are automatically uploaded to cloud-based data repositories for remote monitoring, distance consults, and quality assurance.
Phone-based tools, such as medical apps and subunit attachments, add to the diagnostic armamentarium. Kipuwex, for example, is a wireless Internet of Things (IoT) device that can be used to continuously monitor nine clinical biomarkers vital to the management of high-risk patients (Kipuwex 2020). From ultrasound plug-ins to tuberculosis screening via selfies, smartphones are a powerful enabler of health-tech innovations.
Table: Barefoot Doctor 2.0 Toolkit Weights
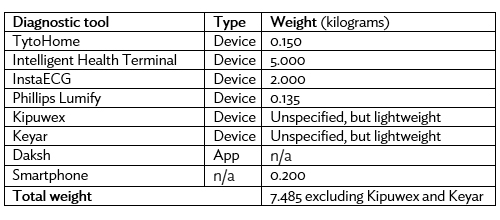
Source: Authors’ calculations.
Making it happen: Practical challenges and considerations
Most of the innovations described here are still in their early stages, largely networked within their respective domestic markets and not yet globally mainstream. Polishing the technology, increasing manufacturing capacities, and lowering prices will be crucial if those tools are to reach the remaining 52% of the world without healthcare. Case in point—at $300, the price of a TytoHome device is 8 times more than the value of annual per-capita healthcare spending in Bangladesh, making it an unrealistic solution for low-resource healthcare settings.
The decision-support component of novel technologies will also have to be strengthened. While various tech innovations have dramatically altered conventional modes of health screening, individual diagnoses and decision-making are largely still left up to physicians, virtual or not. Harnessing the potential of AI will be key to transforming current solutions into truly intelligent systems capable of point-of-care diagnosis. Pie in the sky? No—an AI diagnostic system developed by Babylon Health has already been deployed in multiple health systems across Rwanda and the United Kingdom (see Figure) (Comstock 2018).
Figure: Babylon Health’s Triage Chatbot and Virtual Confirmation Platform
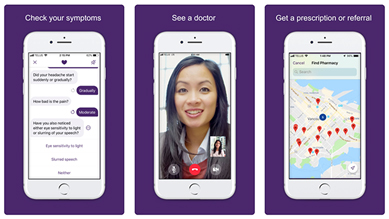
Source: Muoio (2019).
To optimize the predictive accuracy of such algorithms, massive training data sets will have to be obtained on wide demographic spectrums. For this to happen, a universal, low-cost, and secure data ecosystem will be required. Unfortunately, current data sets are mostly disparate and spread across diverse and proprietary siloes. Solutions do exist and there is some optimism—openEHR data platforms have been gaining increasing recognition for their interoperability and vendor-neutrality, the most established being Marand’s Better Platform (Better 2019). The challenge now is to expand this network and integrate the remaining repositories for a single, longitudinal international record.
Health financing also needs to be rethought. Domestic government funds are unlikely to form a realistic starting point given the already-colossal gaps in annual health funding, and leveraging the private sector and philanthropic venture monies will be critical. This will require a nuanced balancing of social and commercial interests, such that public health objectives may be fulfilled while attracting investors.
Can we have our cake and eat it too? Sure, we can. Will philanthropists step up? We would think so—if nothing else, “enlightened self-interest” will motivate. No country is safe from COVID-19 until every country is safe, and it is in the rich world’s interest to assure that health systems in even the poorest countries are functional and resilient.
Would investors smell opportunity? Yes—as the late Harvard business professor CK Prahalad exhorted the world almost 2 decades ago, there is a fortune at the bottom of the pyramid. Poor people, like all peoples, want to live healthy lives, and business models congruent with their purchasing abilities can thrive as the modest unit fees are balanced by the massive numbers.
It is time for “barefoot doctor 2.0” to move into practical reality. The technologies exist, and the needs are real and immediate. Such tech-driven approaches are no longer a luxury—they are a necessity. Neither are they science fiction—they are already happening, just not everywhere.
______
References
Azevedo, M. 2020. Tyto Care Lands $50M To Provide Remote Medical Exams.
Better. 2019. Better Platform.
Comstock, J. 2018. Babylon’s AI Passes Mockup of UK’s GP Exam, Goes Head-to-Head with Doctors. MobiHealthNews.
Dai, S. 2018. A Look at How China Is Using Technology to Improve Rural Access to Quality Health Care. South China Morning Post.
Janitri Innovations. 2020. Products.
Kipuwex. 2020. Professional Use.
Muoio, D. 2019. Babylon’s Triage Chatbot Launches in British Columbia. Mobi Health News.
Sayburn, A. 2020. COVID-19: Is Primary Care Ready to Switch to Telemedicine? Medscape.
Tricog. 2020. InstaECG.
World Health Organization. 2008. China’s Village Doctors Take Great Strides.









Comments are closed.