 Hypertension affects 25% of the world’s population and can be a silent killer with no warning signs (Zhou et al. 2021). The condition is defined as blood pressure that is consistently higher than normal (Joffres et al. 2001). It is particularly prevalent among men in high-income Asia and the Pacific (37.7%), followed by Central Asia and North Africa (36%) and South Asia (32%), while the proportion of diagnosed and treated hypertension among all cases of hypertension for men and women is highest in high-income Asia and the Pacific and lowest in South Asia (Figure 1). Several low- and middle-income countries are currently going through an epidemiological transition, and the global burden of hypertension is rising along with the threat of non-communicable diseases among the youth and the economically active population (Naghavi et al. 2017).
Hypertension affects 25% of the world’s population and can be a silent killer with no warning signs (Zhou et al. 2021). The condition is defined as blood pressure that is consistently higher than normal (Joffres et al. 2001). It is particularly prevalent among men in high-income Asia and the Pacific (37.7%), followed by Central Asia and North Africa (36%) and South Asia (32%), while the proportion of diagnosed and treated hypertension among all cases of hypertension for men and women is highest in high-income Asia and the Pacific and lowest in South Asia (Figure 1). Several low- and middle-income countries are currently going through an epidemiological transition, and the global burden of hypertension is rising along with the threat of non-communicable diseases among the youth and the economically active population (Naghavi et al. 2017).
Figure 1: Hypertension Among Men and Women in Asia, 2019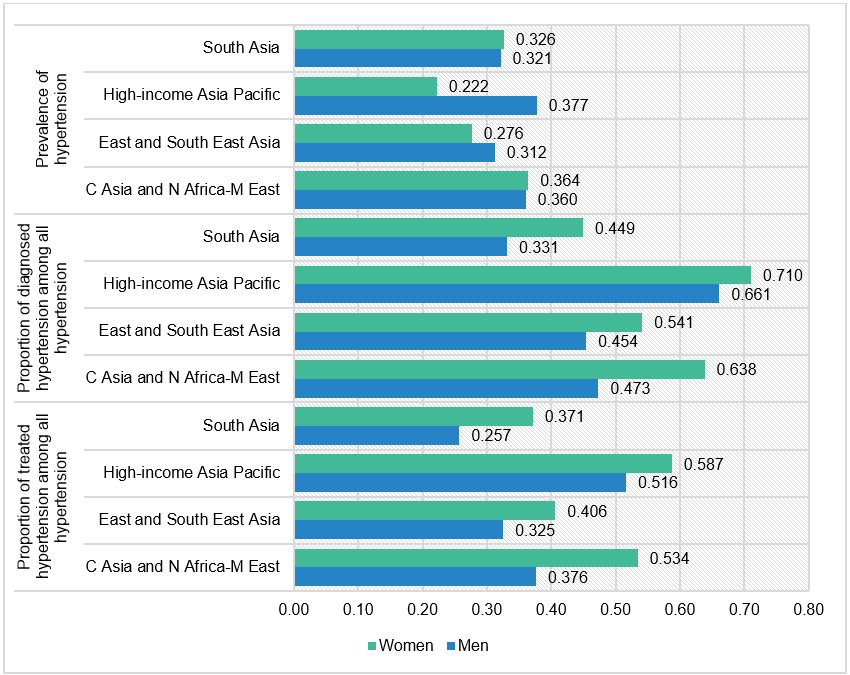 Source: NCDrisC [1] (accessed 14 January 2023).
Source: NCDrisC [1] (accessed 14 January 2023).
Hypertension is generally asymptomatic, and many affected people are unaware they have it. According to the World Health Organization [2], the number of adults with hypertension increased from 594 million in 1975 to approximately 1.3 billion in 2015, mainly in low- and middle-income countries worldwide. This increase was primarily due to a rise in hypertension risk factors due to growth in the global population, aging, and changes in lifestyle and food habits.
Every cloud has a silver lining
Prehypertension is a precursor of hypertension, and independently it has a strong positive linear relationship with cardiovascular disease. Prehypertension eventually leads to hypertension with increasing age, and the share of the young population with the condition is growing in low-and middle-income countries (M. Rahman et al. 2015; A. Rahman et al. 2021).
However, to look on the brighter side, hypertension can be reversed through changes in lifestyle, such as reducing body weight, doing physical exercise, improving dietary patterns, reducing sodium and alcohol consumption, and increasing fruit and vegetable intake (Svetkey 2005). Early detection among younger adults can be achieved through understanding the prevalence of prehypertension (Hasan et al. 2018; Kibria et al. 2021; Ramakrishnan et al. 2019).
Country-specific studies from South Asia show that the prevalence of hypertension is high among residents of urban areas and those from more affluent backgrounds (Biswas et al. 2016; Ghosh and Kumar 2019; A. Rahman et al. 2021). Using Demographic and Health Surveys, Rahut et al. (2022) showed that more than 50% of adults aged 18–49 years old suffer from prehypertension and hypertension in South Asia, with prevalence high among better-educated and wealthy individuals living in urban areas. For instance, the prevalence of prehypertension and hypertension in India is 43.2% and 14.9%, respectively, 35.1% and 19.8% in Bangladesh, and 25.2% and 13.8% in Nepal.
Mechanisms for prevention and management
Hypertension prevention is important as the condition is associated with a decline in quality of life and can exacerbate cardiovascular disease risk. Prehypertension is high and pervasive, but it can be prevented from developing into hypertension if preventive strategies are implemented and feasible. Healthy diets, active lifestyles, and routine blood pressure monitoring are often encouraged, but a mechanism for making such changes is needed, and early detection is key.
Furthermore, ways to accurately measure a patient’s blood pressure are necessary for diagnosing hypertension and assessing comorbid conditions, including stroke, coronary artery disease, heart failure, and peripheral vascular disease. Prevention strategies also call for behavioral mechanisms to be introduced as policy interventions. For management, recommended strategies include reducing and managing stress, regularly checking blood pressure, treating high blood pressure, and managing other medical conditions.
Putting policy in place
Notably, other factors relating to prehypertension are modifiable and can be addressed with appropriate policy transformations. The prehypertension population is an essential indicator to look at. By not letting those with prehypertension become hypertensive, governments can reverse the adverse effects of hypertension. One way to do this is to urgently set up intervention programs operating at multiple levels to increase awareness of hypertension regardless of regional and economic differences. Such interventions include access to high blood pressure treatment via community-wide health programs, such as weight loss and sodium reduction campaigns and home blood pressure measuring programs. These can help to effectively reduce high blood pressure levels and identify those who need medications and treatment. Other effective programs include the self-monitoring of blood pressure levels, and advanced digital technology and its application can make such interventions possible.
In many middle- and low-income countries, prehypertension and hypertension have increased rapidly as awareness, treatment, and control have been minimal and ineffective. Proven solutions to the challenges of hypertension can be adjusted to meet the needs of individuals and communities with different healthcare infrastructure and resources. Enhanced efforts to prevent and treat hypertension are attainable. Pursuing cost-effective approaches that yield substantial health benefits should be a high priority for societies and the public health community, together with behavioral interventions to further introduce evidence-based policy.
References
Biswas, T., M. S. Islam, N. Linton, and L. B. Rawal. 2016. Socio-Economic Inequality of Chronic Non-Communicable Diseases in Bangladesh. PLOS ONE 11, e0167140.
Ghosh, S., and M. Kumar. 2019. Prevalence and Associated Risk Factors of Hypertension Among Persons Aged 15–49 in India: A Cross-Sectional Study. BMJ Open 9, e029714.
Hasan, M., I. Sutradhar, T. Akter, R. Das Gupta, H. Joshi, M. R. Haider, and M. Sarker. 2018. Prevalence and Determinants of Hypertension Among Adult Population in Nepal: Data from Nepal Demographic and Health Survey 2016. PLOS ONE 13, e0198028.
Joffres, M. R., P. Hamet, D. R. MacLean, G. J. L’italien, and G. Fodor. 2001. Distribution of Blood Pressure and Hypertension in Canada and the United States [3]. American Journal of Hypertension 14(11): 1099–1105.
Kibria, G. M. A., R. D. Gupta, and J. Nayeem. 2021. Prevalence, Awareness, and Control of Hypertension Among Bangladeshi Adults: An Analysis of Demographic and Health Survey 2017–18. Clinical Hypertension 27: 1–11.
Naghavi, M., et al. 2017. Global, Regional, and National Age-Sex Specific Mortality for 264 Causes of Death, 1980–2016: A Systematic Analysis for the Global Burden of Disease Study 2016. The Lancet, 390: 1151–1210.
Rahman, A., M. Parvez, H. R. Halder, U. N. Yadav, and S. K. Mistry. 2021. Prevalence of and Factors Associated with Prehypertension and Hypertension Among Bangladeshi Young Adults: An Analysis of the Bangladesh Demographic and Health Survey 2017–18. Clinical Epidemiology and Global Health 12, 100912.
Rahman, M., S. Gilmour, S. Akter, S. K. Abe, E. Saito, and K. Shibuya. 2015. Prevalence and Control of Hypertension in Bangladesh: A Multilevel Analysis of a Nationwide Population-Based Survey. Journal of Hypertension 33: 465–472.
Rahut, D. B., R. Mishra, T. Sonobe, and R. R. Timilsina. 2022. Prevalence of Prehypertension and Hypertension Among the Adults in South Asia: A Multinomial Logit Model. Frontiers in Public Health 10, 5422.
Ramakrishnan, S., et al. 2019. Prevalence of Hypertension Among Indian Adults: Results from the Great India blood Pressure Survey. Indian Heart Journal 71: 309–313.
Svetkey, L. P. 2005. Management of Prehypertension. Hypertension 45: 1056–1061.
Zhou, B., et al. 2021. Worldwide Trends in Hypertension Prevalence and Progress in Treatment and Control from 1990 to 2019: A Pooled Analysis of 1201 Population-Representative Studies with 104 Million Participants. The Lancet 398(10304): 957–980.